ACLM Advocacy Priorities in Support of its Members and Lifestyle Medicine
By Jean Tips, Sr. Director of Communications & Public Affairs
One year after the White House Conference on Hunger, Nutrition and Health, we take a look at ACLM’s advocacy efforts on behalf of our members since we began that work in 2019. Our priority areas of focus are lifestyle medicine in medical education; reimbursement and quality measures; health equity as it relates to lifestyle-related chronic disease health disparities; and military health for recruits and active-duty personnel.
Included in the wide array of American College of Lifestyle Medicine’s member benefits is ACLM’s bipartisan advocacy work on Capitol Hill in support of the integration of lifestyle medicine as the foundation of healthcare and, more specifically, to support our members in their clinical practices. We began our advocacy activities in 2019, initially focused on introductions and orientations with key Congressional members and staff, as well as key representatives of federal agencies such as the Centers for Medicare and Medicaid Services (CMS) and the Department of Health and Human Services (HHS).
As a 501(c)(3) nonprofit organization, ACLM is a tax-exempt entity that is prohibited from engaging in certain types of political activities such as lobbying. However, we can work to influence and provide critical background for federal stakeholders involved in areas of public policy and issues that affect our work. Over the past four years, our priorities have remained the same: 1) advance lifestyle medicine, including food as medicine, in medical and other health professional education, 2) remove reimbursement barriers and improve quality measure misalignment, 3) improve military health as a matter of national security and military preparedness, and 4) foster health equity by addressing lifestyle-related chronic disease health disparities.
We have executed our work with the deft on-the-ground assistance in D.C. of health policy consultants Alston and Bird.
Our ongoing work to date has included a variety of tactics:
- continued introduction, briefing, and relationship management of key legislative champions and their staff, especially those who are members of committees of jurisdiction governing healthcare and key caucuses
- direct origination of responses to requests for information (RFIs) from Congress and federal agencies such as CMS on topics that include the Physician Fee Schedule and Agriculture Improvement Act (the “Farm Bill,”) as well as sign-on to other organizations’ letters related to specific lifestyle-related topics
- identification of, membership in and collaboration on the work of special advocacy-related nonprofits and industry partners (such as the Primary Care Collaborative, Partnership to Fight Chronic Disease, Population Health Alliance, Physical Activity Alliance, Diabetes Advocacy Alliance, and The Root Cause Coalition) and legislation-specific groups (such as the Medical Nutrition Therapy Act Coalition) to amplify efforts with a larger and more influential voice
- support to onsite visits of ACLM member practices for key Congressional staff and agency members
- obtaining “a seat at the table” at key summits and public forums, often comprising ACLM leadership and members providing testimony to present their views and influence reports and decision-making, including for the Dietary Guidelines for Americans 2025-2030
- proposal of lifestyle-medicine language insertion to bills and proposed regulations
- “ear-to-the-ground” scanning of activities and opportunities
- media engagement through op-eds and pitches to raise awareness of lifestyle medicine and its role and relevance in current conversations, in both industry and consumer media outlets
Nutrition in Medical Education
Not long after starting our advocacy work came the COVID-19 pandemic and the glaring public realization of the obvious role chronic disease (“underlying conditions”) played in the worst cases and outcomes of COVID-19, especially among our most vulnerable populations. The “silver lining,” if you will, has been the awareness of the urgent need to address lifestyle-related disease root causes. The cracks in our state of national health were so alarming and the causes so apparent that the phrase “diet-related disease” has become frequently used on Capitol Hill.
With the growing realization of diet’s relationship to chronic disease, and at the urging of Rep. Jim McGovern and others, came last fall’s White House Conference on Hunger, Nutrition and Health, the first of its kind in 50-plus years. It was an advocacy milestone for ACLM and a watershed for visibility.
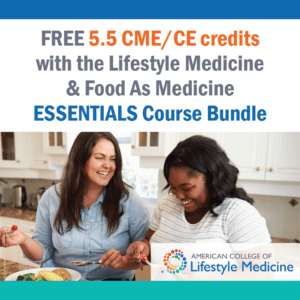
ACLM made a $24.1 million commitment highlighted at that event to provide 5.5-hours of complimentary CME/CE/MOC through our Lifestyle Medicine and Food is Medicine Essentials online course, offered to 100,000 clinicians, and half the cost of certification for one primary care provider in each of our nation’s ~1,400 Federally Qualified Health Centers (FQHCs).
Now a year out from that seminal event, nearly 30,000 clinicians have registered for the course, and state funding partnerships are being launched on the FQHC portion of the commitment, which we now refer to as ACLM’s National Training Initiative . Health systems and insurance companies have offered the course to their employees and networks. ACLM has been invited to multiple stakeholder events organized on the topic of “food as medicine,” something that the College has championed since its inception in 2004, long before COVID or the White House Conference.
Visibility of ACLM on the national stage around our work on the first of our priorities has accelerated to a level far greater than ever expected when we started advocacy four years ago, and the Essentials course commitment has opened invitations to never-expected conversations, meetings, and partnerships. For example, ACLM is forging new partnerships to provide the complimentary course to organizations such as the National Medical Association, American Women’s Medical Association and Association of Clinicians for the Underserved. Other activity has recently included presentations and meetings with the Association of American Medical Colleges (AAMC), Accreditation Council for Graduate Medical Education (ACGME), and American Association of Colleges of Osteopathic Medicine (AACOM).
Now we are doubling down on the commitment, expanding the availability to 200,000 clinicians, extending the opportunity for complimentary registration in this $220 course offering through September 2025. Ongoing post-conference work includes attending monthly progress calls with the White House staff and reporting to the Centers for Disease Control (CDC) Foundation, the agency charged with monitoring all commitments that were made.
Reimbursement
Reimbursement has been a multifaceted priority area focused on the points of pain our members experience in their daily practice of lifestyle medicine, specifically in payment and misalignment of quality measures that affect payment. Lifestyle medicine delivery simply does not fit existing payment and incentive structures, and, in general, there is a lack of incentives to restore a patient’s health.
Overall, fee-for-service (FFS) models do not easily support the delivery, reimbursement or incentivization of intensive lifestyle medicine care by a multi-disciplinary team of clinicians, often in a group-visit environment.
The following are examples of the known issues within the FFS arena that ACLM is committed to addressing through advocacy on behalf of our ALCM members:
- a Relative Value Units (RVU)-based system that pays for volume of care, not for performance/outcomes
- misaligned incentives/quality measures that reward process, focus on pharmaceutical compliance, and penalize health restoration
- Evaluation and Management (E/M) coding and billing that doesn’t fit the longer, multiple visits and shared medical appointments required for behavior change through lifestyle medicine. In fact, billing the same patient for multiple visits creates perceived compliance concerns
- patient co-pays for frequent visits that create a financial burden and modifiers that are not universally covered for prevention much less treatment of disease
- lack of space in offices that are built for 1:1 patient visits and thus curtail shared medical appointments, but place-of-service (POS) requirements that limit access and reimbursement for patients in community settings such as schools, places of worship and teaching kitchens even though these address social influencers of health
- limited or no reimbursement for interdisciplinary care team members such as health coaches, RDNs, exercise physiologists, OTs/PTs, behavioral health professionals and RNs for delivering LM services
On the other hand, while decidedly a better payment model for lifestyle medicine, value-based payment models are not without their challenges. For instance, risk scoring pays providers for taking on high risk patients. But, when a patient gets better (i.e., reverses their chronic disease), the risk score for the patient goes down, and the payment to the provider also goes down. There is not an incentive, and in fact there is a financial penalty, to achieve health restoration for sick patients.
To correct these issues, advocacy will take time, as making changes are complex, bureaucratic, lengthy and, in some cases, financially prohibitive. Awareness among decision-makers of these barriers is a first step, so ACLM is commenting on such issues in requests for information and in meetings and other venues—protocol for being “on the record”—is essential to further action.
Military Health
Recently published research shows the health of our military recruits and active-duty military has deteriorated to the point of being a national security threat. Lifestyle medicine is starting to be integrated, and ACLM has been working with several branches of the military and the VA/DOD through several of our member interest groups and diplomates to make this happen. The interest in lifestyle medicine training and certification within military healthcare has been growing consistently and several large-scale training programs are in development.
Our specific strategy for advocacy is in its early stages, but being discussed as one idea is how to expand the incorporation of our Lifestyle Medicine Residency Curriculum into military residencies, beyond those residency programs already engaged.
Health Equity
ACLM’s federal advocacy for health equity focuses on strategies to provide lifestyle medicine access to historically medically underserved communities and lifestyle medicine knowledge to help underrepresented in medicine clinicians help patients make healthy lifestyle choices that curb lifestyle-related chronic disease health disparities.
These strategies to date have included conversations with health equity champions in Washington, D.C., such as the Congressional Black Caucus and CMS Office of Minority Health in order to introduce them to ACLM, to lifestyle medicine and to the efforts of our HEAL (Health Equity Achieved through Lifestyle Medicine) Initiative. We also are identifying and starting partnership conversations with minority medical associations such as the National Medical Association and National Association of Hispanic Nurses to offer the Essentials course and potentially join forces in advocacy efforts to support their underrepresented in medicine (UIM) members who are often on the front lines of providing care to minority patients.
Other advocacy efforts in support of health equity include participating in opportunities in which we can learn about the policy efforts that align with addressing lifestyle-related chronic disease health disparities in underserved communities. For example, ACLM’s Director of Advocacy and Health Equity Stacia Johnston this year has participated in the Congressional Black Caucus Foundation’s recent Policy for the People Health Equity Summit and CMS’ inaugural Health Equity Conference, which convened policymakers and community stakeholders to discuss ways to address social influencers of health on a federal level to create sustainable impact in historically disadvantaged communities.
ACLM has also supported onsite meetings of Congress members and staff and CMS staff to showcase ACLM members who are doing lifesaving work in communities of need.
FQHCs, which provide invaluable health services to upwards of 30 million patients in vulnerable populations across the country, are ACLM’s new health equity focus area. To learn how to reach FQHC clinicians with lifestyle medicine resources and determine advocacy opportunities, we have met with senior leadership of the Health Resources and Services Administration (HRSA) and the Association of Clinicians for the Underserved (ACU), and exhibited at the National Association of Community Health Centers (NACHC) CHI & Expo, the largest conference for community health center professionals.
Four years into its advocacy work, even if disrupted somewhat by the pandemic, ACLM is making significant progress in influencing those on The Hill to understand the value of lifestyle medicine as the foundation of health and make it easier to practice this high-value care so critical to the success and sustainability of our nation’s healthcare going forward.